Retinal Vein Occlusion (blocked vein)
The Retina is a light-sensitive tissue that lines the inside of the eyeball and transmits the visual information to the brain. Each eye’s retina has one main central vein which branches into numerous smaller retinal vein branches.
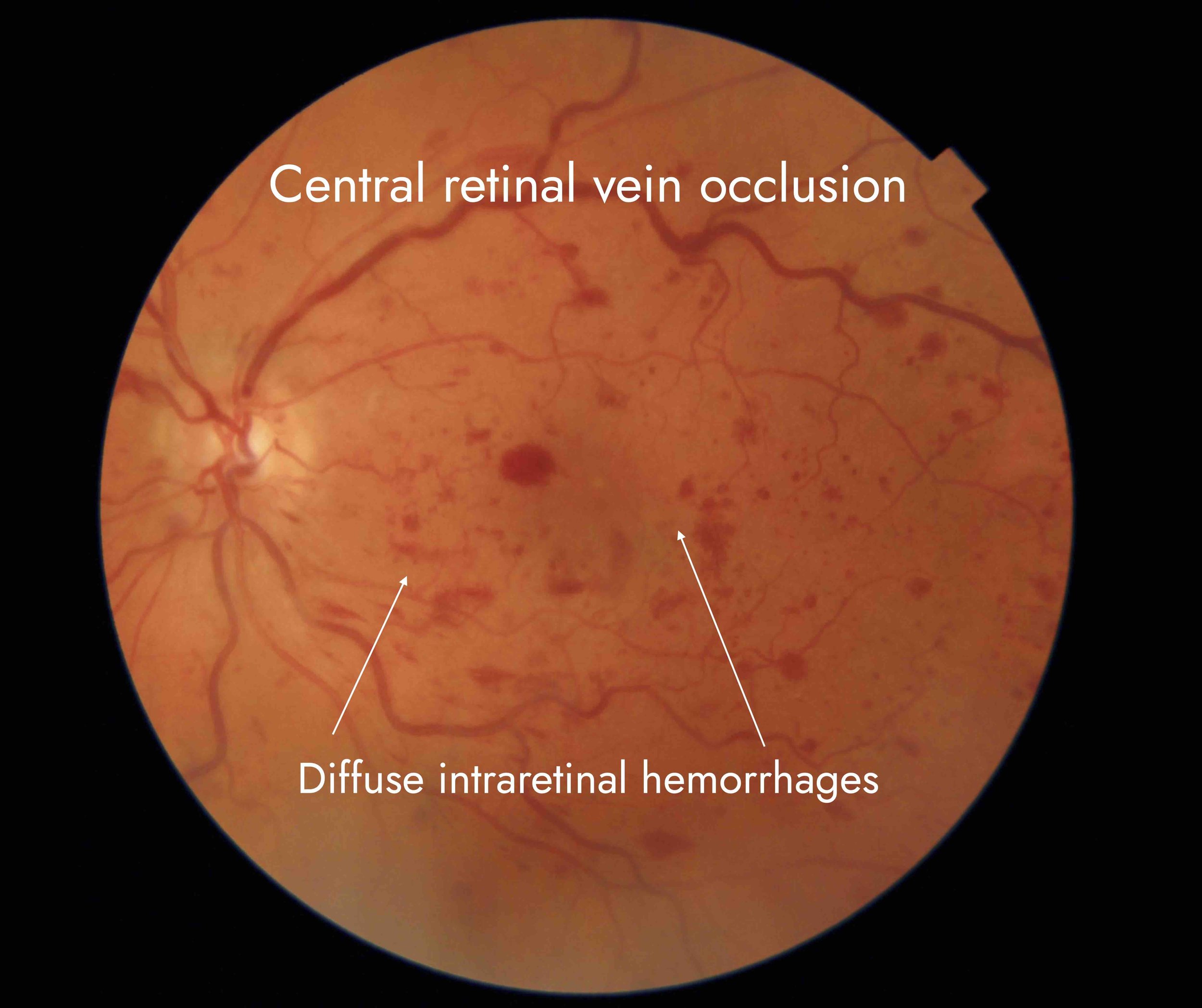
Retinal vein occlusion can affect the main vein (central retinal vein occlusion) or any of the branches. Occlusion (blockage) of the main vein is called a central retinal vein occlusion (CRVO). An occlusion of one of the branches of the vein is called a branch retinal vein occlusion (BRVO).
When a vein is blocked, the area of the retina cannot drain well. This means it can become “boggy” with body fluid and blood collecting within the retina.
This swelling is called retinal oedema. If the swelling affects the centre of the retina called the macula, then this is called macular oedema (swelling of the macula). This condition requires treatment because it affects vision.
Symptoms?
Blurry vision is the most common symptom of retinal vein occlusion. If the central (main) retinal vein becomes blocked, all vision will go blurry on the affected eye. If one of the branches of the vein become blocked, then only part of the vision will go blurry.
This can happen suddenly or become worse over several hours or days. The severity of vision loss can range from a mild blur to profound loss of vision. Some patients may not be aware of any change in the vision. In these cases the vein occlusion may be discovered during a routine eye check.
Other symptoms include dark patches in the vision or rarely floaters. In severe cases, a feeling of pain or pressure in the eye may be experienced. This may occur some months or years following the initial vein blockage.
If the occlusion affects one of the smaller, peripheral branches, the person is usually not aware of any symptoms.
Central Retinal Vein Occlusion (CRVO)
the blockage happens in the larger central vein, which impacts the entire retina
Branch Retinal Vein Occlusion (BRVO)
the blockage happens in one of the smaller retinal veins and only impacts that section of retina
Diagnosis?
Diagnosis and treatment plan are made through ocular examination and advanced diagnostic technology including:
Fluorescein angiogram of a person with diabetes
Heidelberg Spectralis Ocular Coherence Tomography (OCT)
OCT Angiography
Fundus Fluorescein Angiography
When you arrive for your appointment, you will be asked about your symptoms. Our doctors will check your vision and eye pressure. You will then have a series of scans to evaluate your retina and the veins in your eye in great detail. Your eye specialist will examine the eyes through dilated pupils and will explain the findings and the treatment options. Some patients may need to have a blood test.
Causes?
Conditions that affect blood vessels, such as high blood pressure, diabetes, blood clotting disorders and smoking are risk factors for a vein occlusion.
Why is my vision reduced?
There are several effects of a blocked vein
Numerous haemorrhages occur in the affected part of the retina. These can be seen as dark blotches in the vision
The retina swells because the vein which drains the blood is not working
If the blockage is severe, the blood supply is too poor for that part of the retina to continue to function.
If there is no blood supply, the eye can grow new blood vessels which rather than helping the circulation, can cause severe complications such as bleeding in the eye or glaucoma.
Treatment?
A blocked vein cannot be unblocked. It is up to your remaining circulation to support the recovery of the eye. The treatment is aimed at helping this process and preventing/ treating complications of the vein occlusion, such as growth of new abnormal blood vessels. Treatment will be individually tailored to you and may involve:
Observation only if the vein occlusion is an incidental finding picked up during routine eye examination and the vision is not affected
Injections if the retinal swelling is affecting the vision or causing structural damage. Injections are given every month initially, then depending on the swelling. Most patients who do develop recurrent retinal swelling will require on average 7-8 injections in the first year of treatment, 4-5 injections in the second year and fewer still later on. Some patients may only need a few injections. The amount of swelling and therefore the treatment duration will depend on how well the remaining circulation kicks in.
Laser is sometimes used to improve the swelling, but more often it is used to prevent or treat the growth of abnormal blood vessels
The cost of treatment may be covered by your help fund
If the vision is not affected, the blockage of the vein is mild and the underlying circulation is good. The eye will need to be checked regularly but treatment is usually not needed.
If the vision is affected by the swelling of the macula, treatment is almost always needed. The swelling of the macula is usually treated with injections of a special medication. The medication dries up the swelling and supports the eye while the circulation is recovering. We offer three different types of to suit our patients’ individual needs. Your ophthalmologist will discuss the risks and benefits of the treatments with you.
Most people will notice an improvement in the vision once the macula is dry. It is usual to need a number of injections while the eye is recovering from a vein occlusion. Some patients recover after only a few injections, while some need injections for many years. Usually, the frequency and the number of the injections will decrease as time goes on.
Although laser can occasionally be used to treat retinal swelling, it is usually reserved for severe cases of vein occlusions where a large area of retina is not getting enough oxygen. This can result in the growth of new, damaging blood vessels that can cause bleeding and high eye pressure.
Prognosis
Prognosis depends on the extent and the location of damage caused by the vein occlusion. Your ophthalmologist will be able to assess this from the scans you will be having.
Generally, the better the starting vision, the better is the circulation in the eye and therefore, the better the prognosis. Most people who have macular oedema but relatively good underlying circulation will find that their vision gradually improves after the injection. It is common to receive three injections, one every month, to give the circulation the best chance to recover. If the blood vessels are still leaking, further injections will be needed.
If the blood supply is poor and the retina is unable to get enough oxygen, the retinal cells will begin to die, resulting in a patch of blurry or gray vision.
Lack of oxygen to the retina can result in growth of abnormal blood vessels in the eye that can cause bleeding inside the eye (vitreous haemorrhage) or high pressure in the eye (neovascular glaucoma). This can happen months or years after the vein occlusion and it is therefore important that those at risk have ongoing follow up. Your doctor will be able to determine your risk based on your clinical examination and the tests you will be having.
Reducing the risk of vein occlusion in the other eye
High blood pressure is the biggest risk factor for the development of a vein occlusion. Other risks include:
Heart disease
Obesity
Glaucoma
Smoking
To reduce the risk of vein occlusion, you should:
See your GP to have your cardiovascular risk factors checked
Eat a healthy diet
Not smoke
Exercise regularly